Revisión bibliográfica
- La más clave y última bibliografía sobre OC y aborto
- Donado por Rebecca Cook, Universidad de Toronto
- Actualizada por REDAAS
¿Qué es la objeción de conciencia?
A objeção de consciência possibilita assegurar direitos médicos, mas é um entrave para a saúde pública no Brasil.
Al momento de reflexionar acerca de las posibilidades de acceso a una interrupción voluntaria del embarazo, toma centralidad la figura jurídica de la objeción de conciencia (OC), que en los hechos significa un obstáculo para quienes buscan acceder a su derecho al aborto. “Negarse a cumplir con una obligación legal que revindica los derechos sexuales y reproductivos y la libertad reproductiva de los cuerpos que tienen la posiblidad de gestar se traduce en un obstáculo al acceso de la práctica, pero también tiene la potencialidad de perpetuar las estigmatizaciones en contra del ejercicio del aborto como derecho. Estigmatizaciones que se proyectan también al personal sanitario dispuesto a cumplir con sus deberes legales”, sostiene la autora. Por eso considera que se torna imposible catalogar a la objeción de conciencia “como un acto puramente inmerso en el fuero interno de quien la ejerce, y exige una mirada contextual de la temática. Sobre todo, en sociedades con fuerte impronta religiosa y neconservadora como la cordobesa”.
Luego de 99 años, se modificó el régimen jurídico del aborto. En diciembre del 2020, el Congreso argentino aprobó la Ley 27.610 que reconoce el derecho al aborto hasta la semana 14 inclusive (interrupción voluntaria del embarazo -IVE) y en el momento en que sea necesario en casos de violación y de peligro para la vida o la salud de la gestante (interrupción legal del embarazo -ILE).1 Esta ley regula, además, la atención posaborto. Se trata de una norma de orden público aplicable en todo el país. De este modo, se institucionaliza un cambio de paradigma, abandonándose el que se centraba en la política criminal para adoptar uno basado en derechos y obligaciones, con una visión de salud pública.

The Constitutional Court of Colombia has issued a decision of international significance clarifying legal duties of providers, hospitals, and healthcare systems when conscientious objection is made to conducting lawful abortion. The decision establishes objecting providers’ duties to refer patients to non-objecting providers, and that hospitals, clinics, and other institutions have no rights of conscientious objection. Their professional and legal duties are to ensure that patients receive timely services. Hospitals and other administrators cannot object, because they do not participate in the procedures they are obliged to arrange. Objecting providers, and hospitals, must maintain knowledge of non-objecting providers to whom their patients must be referred. Accordingly, medical schools must adequately train, and licensing authorities approve, non-objecting providers. Where they are unavailable, midwives and perhaps nurse practitioners may be trained, equipped, and approved for appropriate service delivery. The Court’s decision has widespread implications for how healthcare systems must accommodate conscientious objection and patients’ legal rights.

Ramón Michel, Agustina. Video: Aborto no punible: desafíos en la aplicación del fallo de la Corte y debate sobre objeción de conciencia. Julio 2014.
Link para acceder a los videos:
http://fueradelexpediente.com.ar/tag/objecion-de-conciencia/
Marcelo Alegre «Objeción de conciencia y salud sexual y reproductiva». Hoja Informativa. Despenalización. org. 2009.
¿Cómo se aborda la objeción de conciencia?

Conscientious objections (CO) can be disruptive in a variety of ways and may disadvantage patients and colleagues who must step-in to assume care. Nevertheless, nurses have a right and responsibility to object to participation in interventions that would seriously harm their sense of integrity. This is an ethical problem of balancing risks and responsibilities related to patient care. Here we explore the problem and propose a nonlinear framework for exploring the authenticity of a claim of CO from the perspective of the nurse and of those who must evaluate such claims. We synthesized the framework using Rest’s Four Component Model of moral reasoning along with tenets of the International Council of Nursing’s (ICN) Code of Ethics for Nurses and insights from relevant ethics and nursing ethics literature. The resulting framework facilitates evaluating potential consequences of a given CO for all involved. We propose that the framework can also serve as an aid for nurse educators as they prepare students for practice. Gaining clarity about the sense in which the concept of conscience provides a defensible foundation for objecting to legally, or otherwise ethically, permissible actions, in any given case is critical to arriving at an ethical and reasonable plan of action.

Sometimes healthcare professionals conscientiously refuse to treat patients despite the patient requesting legal, medically indicated treatments within the professionals’ remit. Recently, there has been a proliferation of views using the concept of public reason to specify which conscientious refusals of treatment should be accommodated. Four such views are critically assessed, namely, those of Robert Card, Massimo Reichlin, David Scott, and Doug McConnell. This paper argues that McConnell’s view has advantages over the other approaches because it combines the requirement that healthcare professionals publicly justify the grounds of their conscientious refusals of treatment with the requirement that those grounds align with minimally decent healthcare. This relatively restrictive approach accommodates conscientious refusals from minimally decent healthcare professionals while still protecting good healthcare, the independence of the healthcare professions, and the fiduciary relationships.
The past decade has seen a burgeoning of scholarly interest in conscientious objection in healthcare. While the lit- erature to date has focused primarily on individual healthcare practitioners who object to participation in morally controversial procedures, in this article we consider a different albeit related issue, namely, whether publicly funded healthcare institutions should be required to provide morally controversial services such as abortions, emergency con- traception, voluntary sterilizations, and voluntary euthanasia. Substantive debates about institutional responsibility have remained largely at the level of first-order ethical debate over medical practices which institutions have refused to offer; in this article, we argue that more fundamental questions about the metaphysics of institutions provide a neglected avenue for understanding the basis of institutional conscientious objection. To do so, we articulate a met- aphysical model of institutional conscience, and consider three well-known arguments for undermining institutional conscientious objection in light of this model. We show how our metaphysical analysis of institutions creates difficulties for justifying sanctions on institutions that conscientiously object. Thus, we argue, questions about the metaphysics of institutions are deserving of serious attention from both critics and defenders of institutional conscientious objection.
Institutional objection (IO) occurs when institutions providing health care claim objector status and refuse to provide legally permissible health services such as abortion. IO may be regulated by sources including law, ethical codes and policies (including State and local/institutional policies). We conducted a mixed-methods narrative review of the empirical evidence exploring IO to abortion provision globally, to inform areas for further research. MEDLINE (Ovid), Embase (Ovid), CINAHL (EBSCO), Global Health (CAB Abstracts), ScienceDirect and Scopus were searched in August 2021 using keywords including ‘conscientious objection’, ‘faith-based organizations’, ‘religious hospitals’ and ‘abortion’. Eligible research focused on clinicians’ attitudes and experiences of IO to abortion. The 28 studies included in the review were from nine countries: United States (19), Chile (2), Turkey (1), Argentina (1), Australia (1), Colombia (1), Ghana (1), Poland (1) and South Africa (1). The analysis demonstrated that IO was claimed in a range of countries, despite different legislative and policy frameworks. There was strong evidence from the United States that clinicians in religious healthcare institutions were less likely to provide abortions and abortion referrals, and that training of future abortion providers was negatively affected by IO. Qualitative evidence from other countries showed that IO was claimed by secular as well as religious institutions, and individual conscientious objection could be used as a mechanism for imposing IO. Further research is needed to explore whether IO is morally justified, how decisions are made to claim IO, and on what grounds. Finally, appropriate models for regulating IO are needed to ensure the protection of women’s access to abortion. Such models could be informed by those used to regulate IO in other contexts, such as voluntary assisted dying.

We argue that, in certain circumstances, doctors might be professionally justified to provide abortions even in those jurisdictions where abortion is illegal. That it is at least professionally permissible does not mean that they have an all-things-considered ethical justification or obligation to provide illegal abortions or that professional obligations or professional permissibility trump legal obligations. It rather means that professional organisations should respect and indeed protect doctors’ positive claims of conscience to provide abortions if they plausibly track what is in the best medical interests of their patients. It is the responsibility of state authorities to enforce the law, but it is the responsibility of professional organisations to uphold the highest standards of medical ethics, even when they conflict with the law. Whatever the legal sanctions in place, healthcare professionals should not be sanctioned by the professional bodies for providing abortions according to professional standards, even if illegally. Indeed, professional organisation should lobby to offer protection to such professionals. Our arguments have practical implications for what healthcare professionals and healthcare professional organisations may or should do in those jurisdictions that legally prohibit abortion, such as some US States after the reversal of Roe v Wade.
Regulating Conscientious Objection to Legal Abortion in Argentina: Taking intoConsideration Its Uses and Consequences.
Conscientious objection to abortion provision: why context matters

Managing conscientious objection in health care institutions.
HEC fórum, 26(3), 267-283.
La política del camuflaje: la objeción de conciencia como estrategia de la Iglesia Católica.
Instituto Hemisférico de Performance y Política.
Objeción de conciencia y aborto: una perspectiva global sobre la experiencia colombiana. O’Neill Institute for National and Global Health Law.
One understanding of conscience dominates bioethical discussion about conscience. On this view, to have a conscience is to be compelled to act in accordance with one’s own moral values for the sake of one’s “integrity,” where integrity is understood as inner or psychological unity. Conscience is deemed valuable because it promotes this quality. In this paper, I describe the dominant view, attempt to show that it is flawed, and sketch a positive alternative to it. In my opinion, conscience often fails to promote inner unity (regardless of the degree of inner unity we have in mind); acting with a conscience leaves many people broken rather than unified. A better view about the value of conscience is that having a conscience encourages morally responsible agency. My goal is to prove that this alternative explains better what it means to value conscience in health care and the extent to which we ought to value it.

Doing ‘good medical ethics’ requires acknowledgment that it is often practised in non-ideal circumstances! In this article I present the distinction between ideal theory (IT) and non-ideal theory (NIT). I show how IT may not be the best solution to tackle problems in non-ideal contexts. I sketch a NIT framework as a useful tool for bioethics and medical ethics and explain how NITs can contribute to policy design in non-ideal circumstances. Different NITs can coexist and be evaluated vis-à-vis the IT. Additionally, I address what an individual doctor ought to do in this non-ideal context with the view that knowledge of NITs can facilitate the decision-making process. NITs help conceptualise problems faced in the context of non-compliance and scarcity in a better and more realistic way. Deciding which policy is optimal in such contexts may influence physicians’ decisions regarding their patients. Thus, this analysis—usually identified only with policy making—may also be relevant to medical ethics. Finally, I recognise that this is merely a first step in an unexplored but fundamental theoretical area and that more work needs to be done.

Una propuesta regulatoria a partir de de las prácticas de aborto legal en Argentina
En este trabajo sobre OC a la ILE en Argentina, nos enfocamos en dos aspectos fundamentales e interdependientes: la reconceptualización de este fenómeno y una propuesta para regularla en el marco de una política pública de salud. Ambas empíricamente informadas; además de fuentes secundarias, obtuvimos opiniones y percepciones de una encuesta que realizamos a 269 integrantes del sistema de salud pública y 11 entrevistas semiestructuradas a gestorxs y jefxs de servicios también del sistema público de salud, sobre las formas que adquiere la OC, sus causas e impacto.
Este documento se terminó de escribir en agosto de 2018 en el marco del Proyecto Objeción de conciencia: formas, problemas y respuestas frente al aborto legal en Argentina (CEDES-IPAS).
Yes we can! Successful examples of disallowing ‘conscientious objection’ in reproductive health care (Fiala et al)
Physicians, Not Conscripts — Conscientious Objection in Health Care (Stahl y Emanuel)

A widespread assumption has taken hold in the field of medicine that we must allow health care professionals the right to refuse treatment under the guise of ‘conscientious objection’ (CO), in particular for women seeking abortions. At the same time, it is widely recognized that the refusal to treat creates harm and barriers for patients receiving reproductive health care. In response, many recommendations have been put forward as solutions to limit those harms. Further, some researchers make a distinction between true CO and ‘obstructionist CO’, based on the motivations or actions of various objectors. This paper argues that ‘CO’ in reproductive health care should not be considered a right, but an unethical refusal to treat. Supporters of CO have no real defence of their stance, other than the mistaken assumption that CO in reproductive health care is the same as CO in the military, when the two have nothing in common (for example, objecting doctors are rarely disciplined, while the patient pays the price). Refusals to treat are based on non-verifiable personal beliefs, usually religious beliefs, but introducing religion into medicine undermines best practices that depend on scientific evidence and medical ethics. CO therefore represents an abandonment of professional obligations to patients. Countries should strive to reduce the number of objectors in reproductive health care as much as possible until CO can feasibly be prohibited. Several Scandinavian countries already have a successful ban on CO.

Lauren R. Fink, Kaitlyn K. Stanhope, Roger W. Rochat and Oscar A. Bernal. “The Fetus Is My Patient, Too”: Attitudes Toward Abortion and Referral Among PhysicianConscientious Objectors in Bogotá, Colombia. International Perspectives on Sexual and Reproductive Health IternationalPerspectives on Sexual and Reproductive Health, Guttamacher Institute (2016)
Christian Fialaa and John H. Arthur. ‘‘Dishonourable disobedience’’ — Whyrefusal to treat in reproductive healthcareis not conscientious objection. Woman – Psychosomatic Gynaecology and Obstetrics (2014).
Lisa H. Harris. Reconocer las motivaciones de conciencia en la prestación del aborto. N Engl J Med 2012; 367:981-983 Septiembre 13, de 2012 (traducido al castellano por integrantes del Ministerio de Salud de la provincia de Santa Fe y el CEDES).
In this paper we extend Heidi Hurd’s “correspondence thesis” to the termination of pregnancy debate and argue that the same reasons that determine the permissibility of abortion also determine the justifiability of acts involving conscientious objection against its performance. Essentially, when abortion is morally justified, acts that prevent or obstruct it are morally unjustified. Therefore, despite conscientious objection being legally permitted in some global south countries, we argue that such permission to conscientiously object would be morally wrong in cases of morally justifiable termination of pregnancy. After presenting and defending our “correspondence argument” we suggest that conscientious objection should be denied as a matter of public health policy in developing counties, even in cases where adequate referral services are possible. Towards the end, we extend our argument to midwives, nurses, and prospective students in the field. Given their essential position in resource-poor contexts; they too have no claim to conscientious objection.

Conscientious Objection arises as a response to a regulation that is judged as immoral. Faced with a law that is considered unfair, the citizen can respond accepting it against his will, exercising conscientious objection on a personal level or, collectively reaching civil disobedience or revolutionary violence. This is an old discussion known since ancient Greece. The current enactment of laws that allow actions previously judged as crime, and that contravene medical tradition, reactivated the discussion about such objection. Some people, such as Savolescu, who denies the legitimacy of conscientious objection invoked by doctors, arguing that it is inefficient, leads to inequality and is inconsistent. He proposes that the values of these professionals can be tolerated privately but should not be determinant in the public sphere. These arguments are critically examined, mentioning pertinent answers from theoretical and practical points of view. We highlight that ethics should not differ in public and private spheres and the principles should be the same, but exercised in different fields. It is concluded that conscientious objection is acquiring legitimacy and that it is necessary to reflect on the underlying reasons that lead to invoke it. It should be considered a civilized resource against determinations of power that are considered to be an attempt against personal values and moral integrity.
¿Cómo se regula la objeción de conciencia?
En el presente artículo, proponemos una visión interdisciplinaria para abordar el problema de la objeción de conciencia de los profesionales sanitarios en el contexto de la sentencia de la A.I. 54/2018. La hipótesis de la que partimos es que el contenido de esta sentencia se vuelve una fuente de derecho, que sin ser la letra de la ley por sí misma, renueva una discusión legislativa que se encontraba estancada entre posturas aparentemente irreconciliables al establecer una caracterización y limitación de la objeción frente al derecho al acceso a servicios de salud. A lo largo del presente artículo se explicará el papel de la sentencia dentro de la actual discusión legislativa, como los alcances de un derecho a la objeción de conciencia pueden explicarse mediante las teorías de Borowski y Wellman. Finalizando con la influencia que han tenido autores como Giubilini dentro de la postura de la Comisión Nacional de Bioética y proponiendo a la visión de Card como un abordaje novedoso respecto a este problema
Mediante el presente artículo se compara el abanico de argumentos delineados por los máximos órganos de justicia constitucional de Colombia y Chile, respecto a la figura de la objeción de conciencia ante la legalización de las interrupciones de embarazos. De esta manera, se permite vislumbrar las divergencias que el contenido y alcance de la desobediencia toma en la región y la importancia de estos casos como construcciones judiciales sobre las que proyectar definiciones ante el aborto legal de países que comparten el mismo sistema internacional de derechos humanos.
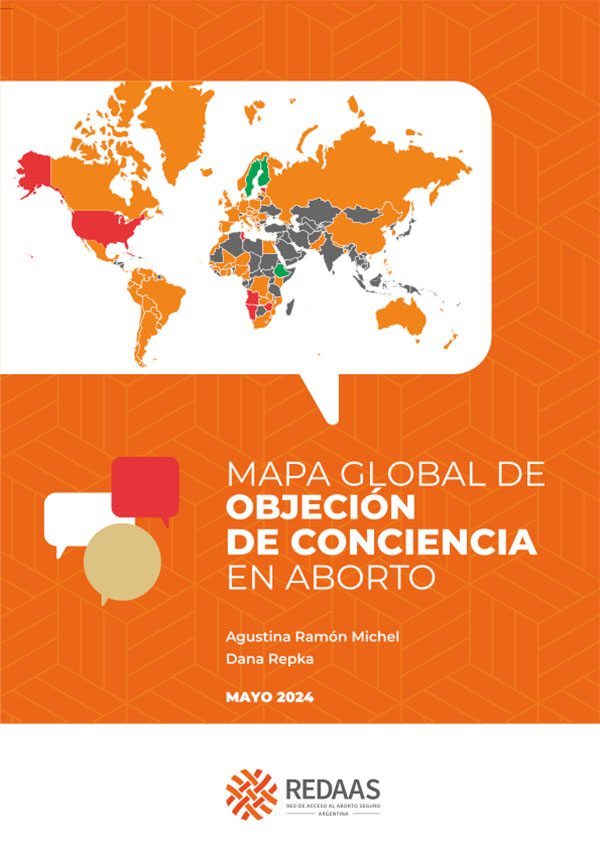
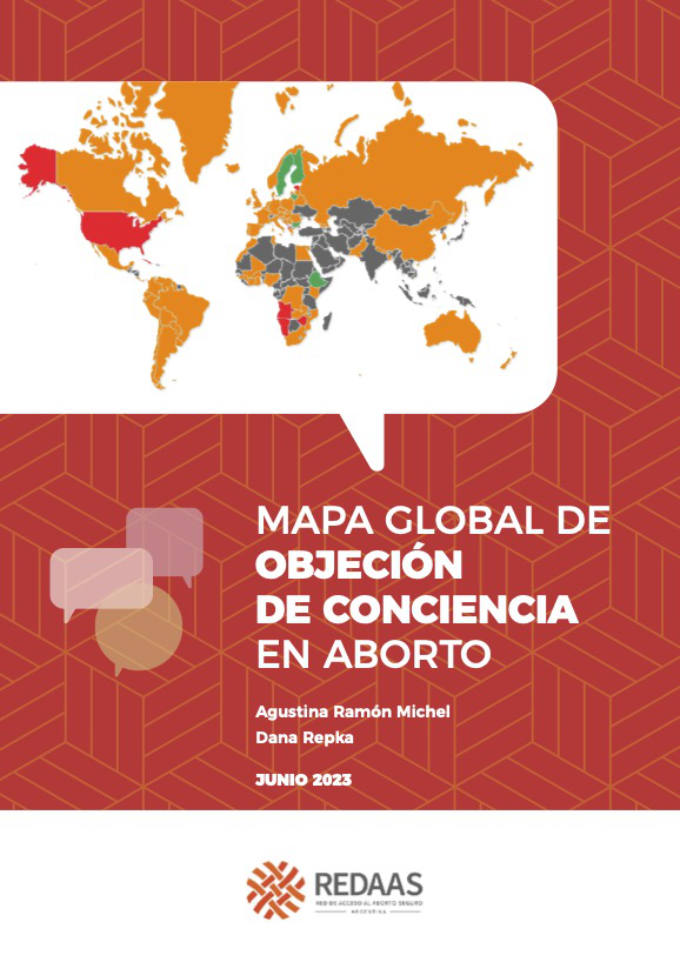
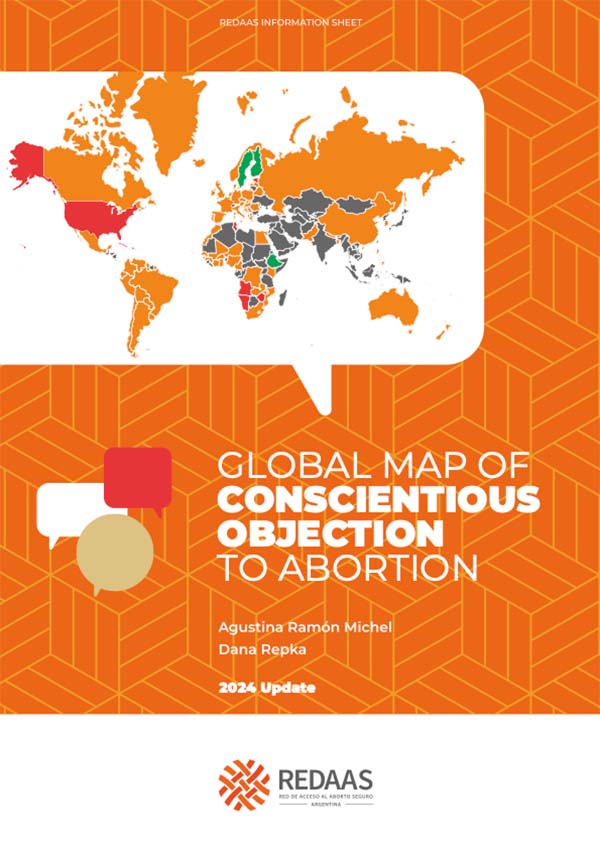
Ya está disponible la hoja informativa “Mapa global de normas de objeción de conciencia”, un trabajo en el que Agustina Ramón Michel y Dana Repka analizan las tendencias a nivel global en materia de Objeción de Conciencia (OC) en aborto.
El Mapa de Normas sobre Objeción de Conciencia en Aborto es un proyecto que cuenta con el apoyo de Ipas Latinoamérica y Caribe. Se trata de un mapa interactivo, online e inédito que releva, analiza y compara cómo los países regulan la OC en la atención del aborto.
¿Sabías que solo 5 países en todo el mundo prohíben la Objeción de Conciencia de manera explícita? Este y otros datos sobre OC en atención del aborto los encontrás en este trabajo.
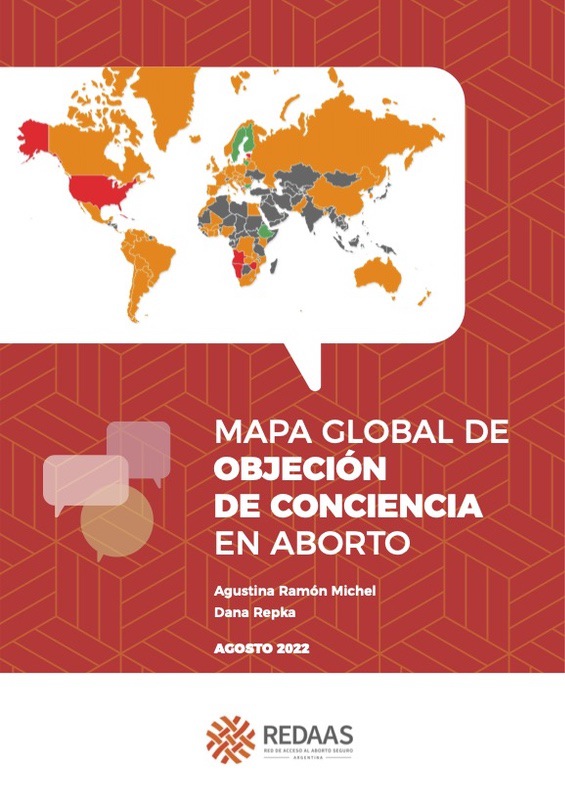
Ya está disponible la hoja informativa “Mapa global de normas de objeción de conciencia”, un trabajo en el que Agustina Ramón Michel y Dana Repka analizan las tendencias a nivel global en materia de Objeción de Conciencia (OC) en aborto.
El Mapa de Normas sobre Objeción de Conciencia en Aborto es un proyecto que cuenta con el apoyo de Ipas Latinoamérica y Caribe. Se trata de un mapa interactivo, online e inédito que releva, analiza y compara cómo los países regulan la OC en la atención del aborto.
¿Sabías que solo 5 países en todo el mundo prohíben la Objeción de Conciencia de manera explícita? Este y otros datos sobre OC en atención del aborto los encontrás en este trabajo.
The first English version of the Global Map of Norms regarding Conscientious Objection was released on April 7. This is an online map that systematizes legal sources on Conscientious Objection (CO) to abortion from more than 180 countries and other administrative agencies worldwide, a research carried out by Agustina Ramón Michel and Dana Repka (CEDES). Social science scholars, health providers, lawyers and activists from Argentina, the United States, Italy, Mexico, South Africa, and FIGO experts on CO came together to discuss the topic. Space for main ideas, data, and discussions.
El 7 de abril se lanzó la primera versión en inglés del Global Map of Norms regarding Conscientious Objection, mapa online que sistematiza las fuentes legales en materia de Objeción de Conciencia (OC) en aborto de más de 180 países y otras dependencias administrativas del mundo, investigación llevada adelante por Agustina Ramón Michel y Dana Repka (CEDES). Se reunió a académicas de ciencias sociales, proveedores de salud, abogadas y activistas de Argentina, Estados Unidos, Italia, México y Sudáfrica, y de FIGO expertas en OC para conversar sobre el tema.

The right to sexual and reproductive health (SRH) is an essential part of the right to life, the right to health, the right to education and the right to equality and non-discrimination. Access to SRH services is a critical component of enabling women and girls to achieve the highest standards of health and wellbeing.
Tensions between ethics and the law: examination of a legal case by two midwives invoking a conscientious objection to abortion in Scotland.

Proposal to inform European institutions regarding the regulation of conscientious objection to abortion.
The European Journal of Contraception & Reproductive Health Care, 21(3), 198-200.
Conscientious objection to sexual and reproductive health services: international human rights standards and European law and practice.
European Journal of Health Law, 19(3), 231-256.
Negación de servicios por razones de conciencia: documento de posición

Regulation of Conscientious Objection to Abortion
An International Comparative Multiple-Case Study
Since abortion laws were liberalized in Western Europe, conscientious objection (CO) to abortion has become increasingly contentious. We investigated the efficacy and acceptability of laws and policies that permit CO and ensure access to legal abortion services. This is a comparative multiple-case study, which triangulates multiple data sources, including interviews with key stakeholders from all sides of the debate in England, Italy, Norway, and Portugal. While the laws in all four countries have similarities, we found that implementation varied. In this sample, the ingredients that appear necessary for a functional health system that guarantees access to abortion while still permitting CO include clarity about who can object and to which components of care; ready access by mandating referral or establishing direct entry; and assurance of a functioning abortion service through direct provision or by contracting services. Social attitudes toward both objection and abortion, and the prevalence of CO, additionally influence the degree to which CO policies are effectively implemented in these cases. England, Norway, and Portugal illustrate that it is possible to accommodate individuals who object to providing abortion, while still assuring that women have access to legal health care services.
Ana Bejarano Ricaurte y Mariana Castrellón Pérez. Grupo de derecho de interés público. Colección TEXTOS ÚTILES SERIE Documentos de Trabajo Documento de Trabajo 4. Bogotá Agosto de 2013.
El documento retoma los argumentos de la Corte Constitucional de Colombia sobre la inadmisibilidad de la objeción de conciencia institucional.
Purpose: The article aims to elaborate on two recent European Court of Human Rights (ECtHR) decisions which have rejected, on grounds of non-admissibility, the appeals by two Swedish mid- wives who refused to carry out abortion-related services, basing their refusal on conscientious objection, and to expound upon the legal and ethical underpinnings and core standards applied to the framing process of such a ECtHR decision.
Materials and Methods: By drawing upon relevant recommendations from international institu- tions, the authors have aimed to assess how the ECtHR rationale could affect the balance between CO and patient rights; searches have been conducted up until December 2020.
Results: In both decisions the European Court has asserted that the right to exercise conscientious objection must give way to the protection of the right to health of women seeking to have an abortion.
Conclusions: ECtHR judges concluded that the failure to provide for a right to conscientious objection does not constitute, in fact, a violation of the more general right to freedom of thought, conscience and religion, if provided for by a state law to protect the right to health. The legal eth- ical and social ramifications of such a decision are of enormous magnitude.
Medical associations and leading courts reinforce the duty of physicians who con- scientiously object to participating in treatment indicated for their patients to refer them to non-objecting practitioners. Ethical and legal duties require continuity of care when physicians withdraw from patients’ treatment on grounds of conscience. The duty to refer might affect gynecologists when their patients request for example, contraceptive means, sterilization, abortion, medically assisted reproductive proce- dures, or gender reassignment. Legislation and leading law courts, notably the UK Supreme Court and Constitutional Court of Colombia, and professional associations such as the College of Physicians and Surgeons of Ontario, have clarified the duty to refer. Physicians are expected to cater their individual conscience to their professional ethical and legal duties, favoring their patients’ choices over their personal objections. Physicians can object to “hands-on” conduct of procedures they find objectionable, but cannot deny referral on grounds of complicity in what other care providers do.
This article explores the approach of international human rights bodies to conscientious objection to abortion, by requiring states to implement mandatory referral mechanisms where conscientious objection is permitted. This, however, represents an inadequate compromise position as many objecting healthcare professionals also object to referral and circumvent those requirements. Furthermore, referral cannot address the broader issues with the overuse and misuse of conscientious objection provisions which obstructs access to abortion services. After considering the harms caused by conscientious objection and suggestions for alternative regulatory responses, this article proposes that the international human rights framework should aim to strike a contextual balance between freedom of conscience and ensuring access to abortion. This new approach should place clearer obligations on states to properly regulate conscientious objection, including obligations to address socio-cultural stereotypes around motherhood and the foetus, which result in widespread conscientious objection.
¿Qué pasa con la objeción en la práctica?
Background: Conscientious objection (CO) in the context of health care arises when a health care professional (HCP) refuses to participate in a certain procedure because it is not compatible with their ethical or moral principles. Refusal to treat in health care includes, in addition to CO, other factors that may lead the HCP not to want to participate in a certain procedure. Therefore, we can say that CO is a form of refusal of treatment based on conscience. Hastened death has become an increasingly reality around the world, being a procedure in which not all HCPs are willing to participate. There are several factors that can condition the HCPs’ refusal to treat in this scenario. Methods: With the aim of identifying these factors, we performed a systematic review, following the PRISMA guidelines. On 1 October 2022, we searched for relevant articles on Pubmed, Web of Science and Scopus databases. Results: From an initial search of 693 articles, 12 were included in the final analysis. Several motivations that condition refusal to treat were identified, including legal, technical, social, and CO. Three main motivations for CO were also identified, namely religious, moral/secular, and emotional/psychological motivations. Conclusions: We must adopt an understanding approach respecting the position of each HCP, avoiding judgmental and discriminatory positions, although we must ensure also that patients have access to care. The identification of these motivations may permit solutions that, while protecting the HCPS’ position, may also mitigate potential problems concerning patients’ access to this type of procedure.

There is a global shortage of health providers in abortion care. Public discourse presents abortion providers as dangerous and greedy and links ‘conscience’ with refusal to participate. This may discourage provision. A scoping review of empirical evidence is needed to inform public perceptions of the reasons that health providers participate in abortion.

In medicine, conscientious objection refers to the refusal of health care professionals to provide
certain services due to ethical, moral, or religious beliefs. Though often unrecognized, the
practice of conscientious objection is commonplace in Illinois, a state with a significant presence
of Catholic hospitals and legal clauses protecting health care professionals who refuse to provide
reproductive care. Contraceptive access in Illinois has become increasingly complicated by
Dobbs v. Jackson Women’s Health Organization, a 2022 U.S. Supreme Court landmark decision
which retracted the previously held federal constitutional right to abortion. This study contributes
to the growing body of literature on conscientious objection to reproductive care by constructing
a landscape of contraceptive access in Illinois after Dobbs. Interviews were conducted with
fifteen health care providers and scholars of various fields in reproductive health. Relevant
themes were analyzed in the context of racial, socioeconomic, and geographical disparities in
contraceptive access. Results reveal the onus of seeking care to be increasingly placed on the
patient, escalating conflicts between religious institutions and state legislation, and heightened
stress in providers at religious institutions. These outcomes have resulted in a greater workload
for reproductive care providers in secular institutions and the muddling of the definition of
conscientious objection. With future threats to contraceptive access potentially looming, the
policies proposed concern lawmakers, providers, and patients alike, as stakeholders in the
effective delivery of reproductive care. Recommendations also address racial, socioeconomic,
and geographical disparities in contraceptive access in hopes of drawing attention to an often-
overlooked barrier to reproductive care access.
Conscientious objection (CO) on the part of healthcare providers is a growing threat to safe abortion access. In South Africa, evidence suggests that this legal clause may be manipulated as a justification for public-sector healthcare providers to exempt themselves from their duties to provide essential reproductive health services as required by national laws and protocols. This qualitative study improves our understanding of the definitions, perspectives, and use of CO among providers, staff, and facility managers in South Africa, and CO’s effect on public-sector abortion availability. Using 18 focus group discussions and 23 in-depth interviews, we examined CO attitudes and behaviours of staff from health facilities that provide abortion care in Gauteng, Limpopo, KwaZulu-Natal, and Eastern Cape Provinces. We find that CO is invoked for a variety of reasons, some unrelated to the legal basis for objection. There have been progressive shifts in attitudes towards abortion over time, but stigma against women and girls who seek abortion remains substantial among staff at facilities providing abortion. Providers who offer abortion services also report high levels of discrimination and isolation from colleagues. Such factors, combined with operational barriers to offering quality abortion care (such as lack of training support or financial incentives) and lack of clarity on CO definitions and procedures, may incentivise some providers to invoke CO inappropriately. Dissemination of national guidelines on CO should be prioritised to reduce ambiguity, and interventions addressing abortion stigma should be considered for all facility staff to safeguard abortion availability in South Africa. DOI: 10.1080/26410397.2023.2184291

In Italy gynecologists can claim consciousness objection when requested to provide abortion; as described
by the latest data analysis, 70% of them decide to not provide this kind of medical procedure. Psycholog-
ical and sociological research studies about abortion are usually related to the construct of “abortion
stigma” and they are mostly focused on women’s experiences rather than on providers’ ones. The present
study tries to understand the subjective perspective of physicians in relation to abortion and to conscious-
ness objection to better understand the emotional dynamics taking part in their workplace and job’s emo-
tional experience. Structured interviews were administered to 19 gynecologists and trainees in Gynecol-
ogy to explore their feelings connected to their work with a focus on voluntary interruption of pregnancy
and the choice of being or not an objector. Since it is an exploratory study, we decided to employ Emo-
tional Text Analysis to analyze the entire textual corpus of interviews to explore their affective symboli-
zation. Statistical multidimensional analyses were conducted to detect thematic domains (clusters) and
latent factors organizing the contraposition between them, considered as a mirror of emotional dynamics
part of the context. We found out five clusters, referring to different emotional dimensions: the represen-
tation of undesired pregnancy as something unmanageable; the role of consciousness objection in defining
physicians’ professional identities; the role of manhood power on women’s pregnancy; the emotional
detachment needed to deal with abortion and the representation of consciousness objection as an instru-
ment of power. All the results are discussed based on the previous literature.

The aim of this study was to explore service providers’ lived experiences with abortion care in the Republic of Ireland following liberalisation in 2018 via public referendum. Data were collected using semi- structured interviews conducted between February 2020 and March 2021. Thirteen interviews were completed with providers who were directly involved in caring for patients accessing liberalised abortion care in the Republic of Ireland. The sample includes six general practitioners, three midwives, two obstetricians, and two nurses. Interpretative phenomenological analysis identified five super-ordinate themes in the providers’ lived experiences: (1) public reactions to liberalised abortion care; (2) lessons from the service implementation; (3) getting involved in abortion care; (4) moments of moral doubt; and (5) remaining committed to the provision of care. Following liberalisation, providers recalled isolated experiences with anti-abortion sentiments, particularly from those who continue to oppose abortion care. They believed that implementation has been mostly successful in delivering a safe, robust, and accessible service in general practice, though identified ongoing challenges in Irish hospitals. Personally, the providers supported access to care and began providing because they perceived a duty to facilitate access to care. Many, however, reported occasional moral doubts about their work. Despite these, none had considered leaving abortion care and all were proud of their work. They said that patients’ stories were a constant reminder about the importance of safe abortion care. Further work is required to ensure that abortion is fully integrated and normalised and that all providers and patients have access to supports. DOI: 10.1080/ 26410397.2023.2216526

This article delves into the dynamics of managing religious diversity within the healthcare field in Argentina. It focuses on the articulations between health practices and individual belief systems among healthcare professionals and users. Applying a comparative approach based on qualitative interviews, we draw conclusions that underscore the imperative of acknowledging the sociocultural diversity within our societies. This recognition is fundamental in cultivating healthcare environments that not only respect users’ diverse worldviews but also healthcare professionals’ religious perspectives. Our findings advocate for incorporating religious diversity management principles in healthcare, emphasizing the development of inclusive approaches in dealing with health, illness, and wellbeing.
To report a study investigating the implementation of the “conscience clause” by practising nurses in two National Health Service Hospital Trusts in the UK.

The United Kingdom’s Abortion Act 1967 has attracted substantial controversy, which has centred not only on the regulation of abortion itself, but also on the extent to which conscientious objection should be permitted. The aim of this study was to examine a range of health-care professionals’ views on conscientious objection and identify the appropriate parameters of conscientious objection to abortion. Gadamer’s hermeneutic was utilised to frame this study. We conducted semi-structured interviews in two UK locations with 18 pharmacists, 17 midwives, 12 nurses and nine doctors, encompassing a mix of conscientious objectors and non-objectors to abortion. A multi-faceted in-depth data analysis led to the development of a hermeneutic of “respecting self and others”. Four major themes of “doing the job”, “entrusting to others”, “acknowledging institutional power” and “being selective” and 18 subthemes contributed to this overarching theme. The complexity of the responses indicates that there is little consistency within and between each profession. They show that participants who were conscientious objectors were accepted by their colleagues and accommodated without detriment to the service, and that in larger hospitals, such as those where our work was carried out, it is possible to be employed in the service areas that include abortion while still being a conscientious objector. Finally, our results indicate that, by respecting of self and others, each profession should be able to accommodate conscience-based objections where individual practitioners seek to exercise them. Conscientious objectors as well as non-objectors have something to contribute to the ongoing development of the maternity and gynaecological services as abortion is only a small part of the work of these services.
While most countries that allow abortion on women’s request also grant physicians a right to conscientious objection (CO), this has proven to constitute a potential barrier to abortion access. Conscientious objection is regarded as an understudied phenomenon the effects of which have not yet been examined in Germany. Based on expert interviews, this study aims to exemplarily reconstruct the processes of abortion in a mid-sized city in Germany, and to identify potential effects of conscientious objection.
The fourth section of the 1967 Abortion Act states that individuals (including health care practitioners) do not have to participate in an abortion if they have a conscientious objection. A conscientious objection is a refusal to participate in abortion on the grounds of conscience. This may be informed by religious, moral, philosophical, ethical, or personal beliefs. Currently, there is very little investigation into the impact of conscientious objection on service users in Britain. The perspectives of service users are imperative in understanding the real-world consequences and potential impact of conscientious objection and should be considered when creating and reviewing policies and guidelines. This research provided a platform for women and those who can become pregnant to share their experiences and opinions at a time when these voices are largely excluded in the great tradition of Western political philosophy and law-making processes.

The World Health Organization (WHO) and international human rights bodies have long urged states to take steps to ensure that ‘conscientious objection’ does not undermine access to abortion in practice. This review uses an established methodology to identify and integrate evidence of the health and human rights impacts of the practice of conscientious objection/refusal. The evidence identified in this review suggests strongly that conscientious objection negatively affects the rights of abortion seekers and has negative implications for the rights of non-objecting health workers. This is exacerbated in situations where an exercise of ‘conscience’ goes beyond ‘opting out’ of providing care and extends into seeking to prevent abortion through dissuasion, misinformation, misdirection, delay, and sometimes abuse. The insights from this review suggest that states must take better and further action to centre abortion seekers in the regulation of conscientious objection, and to prevent and ensure accountability for rights-limiting manifestations of conscience that go beyond opting out of direct provision of abortion care in non-emergency settings.

Antecedentes: El mal uso de la objeción de conciencia (OC) es una barrera importante para el acceso a los servicios de interrupción legal del embarazo en muchos países, especialmente en países en América Latina. Examinamos los motivos de la negación de servicios de aborto legal en México y Bolivia e identificamos maneras de mitigar el uso indebido de la OC.
Métodos: Realizamos 34 entrevistas a profundidad y 12 discusiones en grupo focal en dos estados de México y cuatro departamentos de Bolivia. Los resultados fueron codificados y categorizados utilizando un enfoque de análisis temático.
Resultados: La negación de servicios de aborto por OC está muy extendida en los establecimientos de salud en México y Bolivia y se emplea principalmente por razones distintas a las consideraciones morales, religiosas o éticas. Las principales razones para la negación de servicios por OC son la falta de conocimiento sobre las leyes relacionadas con el aborto y el temor a tener problemas jurídicos en la prestación de servicios de aborto. En cambio, la razón principal para proporcionar servicios es cumplir con las leyes pertinentes. Negar servicios por OC impacta negativamente a las personas embarazadas y a los equipos de atención médica, reduce las opciones
Conscientious objection of health care providers: lessons from the experience of the United States
Conscientious objection to abortion, the law and its implementation in Victoria, Australia: perspectives of abortion service providers.
Objeción de conciencia, trabas y aborto en caso de violación: un estudio entre médicos de Brasil.
Reproductive Health Matters, 22(43), 141-148.
La objeción de conciencia (OC) es una figura jurídica excepcional. Es que, como principio general, el sistema jurídico demanda y aspira a la obediencia de las normas por todas las personas obligadas. La OC es este curioso caso donde el Estado permite a una persona exceptuarse de una obligación jurídica, debido a sus convicciones morales, siempre y cuando cumpla con los requisitos, procedimientos fijados y no dañe derechos de terceros. Surgió como una forma de proteger minorías religiosas o culturales, usualmente ignoradas por las previsiones de las leyes.
Es así que existe hoy una disonancia descomunal entre lo previsto por los textos y la práctica: la versión de la OC como acto reflexivo, sincero y humilde de una persona que hace parte de una minoría ha cedido frente a otros usos mucho más problemáticos y mucho menos éticos.

Este artículo examina el fenómeno de la objeción de conciencia (OC) a los servicios de aborto legal en Argentina, Uruguay y Colombia. Basado en relatos obtenidos a través de entrevistas, el análisis toma distancia de aquellos enfocados en diferenciar entre OC y barreras al servicio, o en identificar si las razones de objeción son verdaderas o válidas. Partiendo del hecho de que en muy pocos casos las/los objetoras/es están al tanto de las definiciones legales de la OC, se busca entender los significados que las/los entrevistadas/os le atribuyeron, y desde los cuales organizan su práctica médica, y justifican su negación a prestar servicios de aborto. En los tres países las/los entrevistadas/os se oponían principalmente a que fueran las mujeres quienes tomaran la decisión de qué embarazos interrumpir, y cómo y cuándo hacerlo. Los discursos contingentes a través de los cuales las/os médicas/os construyen las racionalidades de su OC están hechos, sobre todo, de un incuestionado apego al control de los cuerpos con capacidad de gestar; y de entendidos médico-sociales de las mujeres como inexorablemente madres, máquinas de reproducción o soportes vitales de fetos.

Despite abortion being legally available in South Africa after a change in legislation in 1996, barriers to accessing safe abortion services continue to exist. These barriers include provider opposition to abortion often on the grounds of religious or moral beliefs including the unregulated practice of conscientious objection. Few studies have explored how providers in South Africa make sense of, or understand, conscientious objection in terms of refusing to provide abortion care services and the consequent impact on abortion access.

Objeción de Conciencia: Una barrera para acceder a los servicios de aborto en América Latina, IPAS.
Lucia Berro Pizzarossa, “Conscientious Objection or Conscious Oppression?: The Uphill Battle to Access Abortion Services in Uruguay” (OxHRH, 11 September 2015) http://ohrh.law.ox.ac.uk/conscientious-objection-or-conscious-oppression-the-uphill-battle-to-access-abortion-services-in-uruguay (Visitado 15 de septiembre de 2015).
Conscientious objection to provide abortion has been enshrined in laws and policies globally. Insufficient attention has been paid to the direct and indirect ways in which conscientious objection compromises women’s access to a lawful abortion. Using a systematic search strategy, this narrative literature review synthesises the literature exploring conscientious objection’s impact on women’s access to abortion in a range of countries. This narrative literature review builds on an extensive literature review published by Chavkin et al. (2013. Conscientious objection and refusal to provide reproductive healthcare: A white paper examining prevalence, health consequences, and policy responses. International Journal of Gynecology & Obstetrics, 123, S41–S56. https:// doi.org/10.1016/S0020-7292(13)60002-8). Searches were undertaken on the Medline (Ovid), Global Health, CINAHL, Scopus and Science Direct databases. Thirty six papers were included for thematic analysis. Conscientious objection to abortion was found to impact women’s access to abortion at three main levels: the practitioner level, the healthcare system level and the sociocultural environment level. Conscientious objection was found to impact access directly through attempts by health professionals to restrict access, and indirectly by exacerbating pre-existing barriers to access. Further research is required to better quantify the extent to which this impacts women and whether interventions are effective in reducing the barriers that conscientious objection creates and exacerbates.
CONTEXT: In 2017, Chile reformed its abortion law to allow the procedure under limited circumstances. Exploring the views of Chilean medical and midwifery faculty regarding abortion and the use of conscientious objection (CO) at the time of reform can inform how these topics are being taught to the country’s future health care providers.
METHODS: Between March and September 2017, 30 medical and midwifery school faculty from universities in Santiago, Chile were interviewed; 20 of the faculty taught at secular universities and 10 taught at religiously affiliated universities. Faculty perspectives on CO and abortion, the scope of CO, and teaching about CO and abortion were analyzed using a grounded theory approach.
RESULTS: Most faculty at secular and religiously affiliated universities supported the rights of clinicians to refuse to provide abortion care. Secular-university faculty generally thought that CO should be limited to specific providers and rejected the idea of institutional CO, whereas religious-university faculty strongly supported the use of CO by a broad range of providers and at the institutional level. Only secular-university faculty endorsed the idea that CO should be regulated so that it does not hinder access to abortion care.
CONCLUSIONS: The broader support for CO in abortion among religious-university faculty raises concerns about whether students are being taught their ethical responsibility to put the needs of their patients above their own.
Future research should monitor whether Chile’s CO regulations and practices are guaranteeing people’s access to abortion care.
International Perspectives on Sexual and Reproductive Health, 2020, 46(Suppl. 1):25–34; doi: https://doi.org/10.1363/46e0620

Although abortion in Italy is free of charge and legal in a broad set of circumstances, 71% of
gynecologists are registered as conscientious objectors, i.e. they are exempted from performing
abortions for reasons of religious or moral beliefs. To assess whether this practice limits abortion
access, we analyze aggregate regional data on abortion and a dataset of over one million clinical
records of single interventions performed between 2002 and 2016. Results, from both cross-
regional panel data and microdata analysis, suggest that conscientious objection hampers abortion
access at the local level, being a significant driver of a woman’s decision of having an
abortion out of the region of residence and leading to longer waiting times to have one. Conscientious
objection appears to have a stronger impact on women living in lower-income regions
or experiencing other forms of economic disadvantage.
This article sheds light on the increasing rate of conscientious objection in the
healthcare sector. As many international actors suggest, safe abortion guarantees a
more comprehensive protection of women’s sexual and reproductive rights. In this
context, the refusal demonstrated by the health care workers prevents the benefits
correlated with the legalization of abortion from being realized, especially in the
developing countries. More specifically, this article investigates the role of conscientious
objection among the health personnel in South Africa. As supported by the literature,
the abortion reform in South Africa has been highly progressive. However, this
legislation has now been facing a number of legal challenges.
Este artículo examina el fenómeno de la objeción de conciencia (OC) a los servicios de aborto legal en Argentina, Uruguay y Colombia. Basado en relatos obtenidos a través de entrevistas, el análisis toma distancia de aquellos enfocados en diferenciar entre OC y barre- ras al servicio, o en identificar si las razones de objeción son verdaderas o válidas. Partiendo del hecho de que en muy pocos casos las/los objetoras/es están al tanto de las definiciones legales de la OC, se busca entender los significados que las/los entrevistadas/os le atribuyeron, y desde los cuales organizan su práctica médica, y justifican su negación a prestar servicios de aborto. En los tres países las/los entrevistadas/os se oponían principalmente a que fueran las mujeres quienes tomaran la decisión de qué embarazos interrumpir, y cómo y cuándo hacerlo. Los discursos contingentes a través de los cuales las/os médicas/os construyen las racionalida- des de su OC están hechos, sobre todo, de un incuestionado apego al control de los cuerpos con capacidad de gestar; y de entendidos médico-sociales de las mujeres como inexorablemen- te madres, máquinas de reproducción o soportes vitales de fetos.

Proponé un recurso OC
Compartí la investigación, norma jurídica, sentencia o material audiovisual que conozcas sobre objeción de conciencia en nuestro repositorio.